Regenerative Medicine

Regenerative Medicine
Regenerative Medicine involves using the patient’s own cells as a tool for healing. In other words, it focuses on developing therapies to regenerate or reconstruct damaged tissues using healthy tissues from the patient.
The main goal is to restore the function of tissues damaged by injuries or aging, and to accelerate recovery in conditions where conventional treatments are limited or insufficient.
This field of medicine has been perfected in recent years and has revolutionized modern medicine. Additionally, the results are highly beneficial for patients since these are minimally invasive and straightforward procedures, with almost no risks or adverse reactions.
There are various procedures, and at the Gastaldi Orquín Institute of Traumatology, we offer a wide range of treatments for any type of injury.
There are various procedures, and at the Gastaldi Orquín Institute of Traumatology, we offer a wide range of treatments for any type of injury.

Growth factors or platelet-rich plasma (PRP):
In recent years, growth factor therapy has improved significantly, and many patients have already benefited from this technique. One of the fields of medicine where it is being used most rapidly is in Traumatology, to help regenerate muscles, tendons, joints, etc.
Spain is one of the pioneering countries in the development of this therapy. Although it initially started with elite athletes (Rafa Nadal, Kobe Bryant, or numerous soccer players), it has now expanded to all types of patients since the results are highly positive.
Due to its benefits and effectiveness, it is being applied in fields beyond Traumatology, such as Dentistry, Ophthalmology, and Cosmetic Medicine.
Growth factors are natural proteins present in our blood platelets that stimulate the repair of damaged tissues. Platelet Rich Plasma (PRP) is a concentrate of these platelets, obtained from a sample of the patient’s own blood, which is processed to extract and activate these regenerative factors.
PRP is mainly applied in traumatology to treat:
Muscle and tendon injuries (fibrillar ruptures, chronic tendonitis, epicondylitis).
Arthrosis and joint damage (knee, hip, shoulder).
Sports injuries (sprains, plantar fasciitis, rotator cuff tears).
It is also used in other medical fields such as Dentistry (bone regeneration), Ophthalmology (corneal ulcers) and Aesthetic Medicine (facial and hair rejuvenation).
Following recovery, PRP injections are administered immediately. The patient is discharged home and can resume their normal activities. The time it takes to see the results of the injections varies depending on the type of lesion treated.
Blood collection: A small blood sample is taken from the patient (similar to a routine blood test).
Centrifugation: The blood is processed in a centrifuge to separate and concentrate the platelets.
Activation: PRP is activated with substances such as calcium chloride to release growth factors.
Infiltration: It is injected into the injured area guided by ultrasound for maximum precision.
The whole process takes 30-60 minutes and is ambulatory (no hospitalization is required).
Mild cases: 1-2 sessions (with an interval of 4-6 weeks).
Moderate/severe cases: 2-3 sessions (spaced 3-4 weeks apart).
In chronic diseases (advanced osteoarthritis) annual maintenance infiltrations may be recommended.
PRP is safe when using the patient’s own blood, but it can occur:
Local discomfort (mild pain, swelling or bruising at the injection site).
Transient inflammatory reaction (24-48 hours).
Infection (extremely rare if sterile protocols are followed).
No risk of immune rejection or systemic side effects.
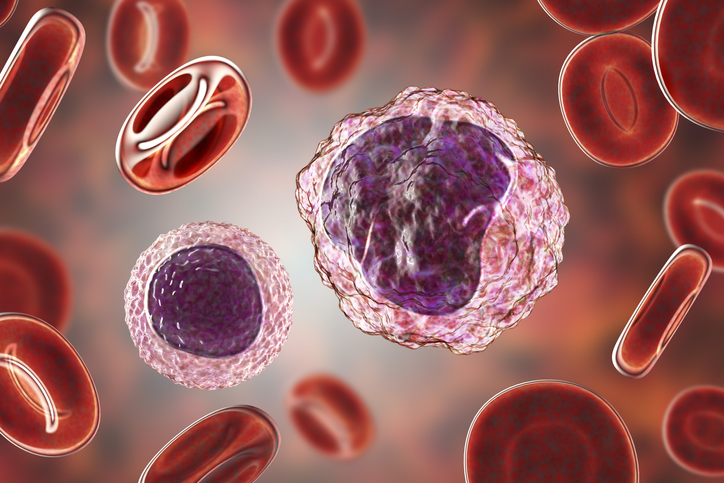
Monocytes
The use of monocytes in biological therapies is an innovative treatment, and has become a promising tool in regenerative medicine and immunology, with the potential to revolutionize the treatment of many diseases. With clinical results equivalent or superior to the use of classical growth factors (PRP).
The monocytes are cells of the innate immune system that circulate in the peripheral blood and migrate to tissues where they become macrophages.
Inflammatory monocytes and tissue-resident macrophages are key regulators of tissue repair, regeneration, and fibrosis. After tissue injury, monocytes and macrophages undergo changes to play critical roles during the initiation, maintenance, and resolution phases of tissue repair.
Monocytes can act as multipotent cells from which bone, cartilage, muscle, or fat can be generated.
In this way, monocytic treatment uses these cells, which are obtained from the patient’s own blood.
Monocytes can be used in virtually any injured tissue. In Sports Traumatology, they are used to aid in the repair of muscle injuries (which are very common), as well as tendon or ligament injuries. In general orthopedics, the most common use is for osteoarthritis.
Following recovery, PRP injections are administered immediately. The patient is discharged home and can resume their normal activities. The time it takes to see the results of the injections varies depending on the type of lesion treated.
To begin with, it is a relatively simple process that takes about 40 minutes. A small amount of blood is drawn from the patient as in a blood test and a special filtering process or apheresis from which a plasma rich in monocytes is obtained.
Subsequently and immediately, the specialized doctor will inject the monocyte concentrate, either directly or through an ultrasound-guided procedure (assisted by an ultrasound machine) to ensure that the growth factors reach the exact location of the injury.
Generally, only a single injection is necessary.
The truth is that, since it is a substance derived from the patient’s own body, no adverse reactions or any type of allergy have been reported.
Mesenchymal Stem Cells
The most biologically valuable tool in the field of regenerative medicine is treatment using mesenchymal stem cells. This therapy allows for tissue regeneration through the use of mesenchymal stem cells. These stem cells can develop into various types of skeletal tissue cells, such as cartilage, bone, and fat. Hence, they are optimal for restoring bodily functions.
Mesenchymal cells are pluripotential cells (“stem” cells) that have the capacity to differentiate into other types of cells of a different cell lineage. That is to say, apart from fat cells or bone marrow cells, we can obtain other types of cells, such as cartilage cells (chondrocytes). This treatment would generate new cartilage cells that regenerate the damaged cartilage lesion.
They can be used in virtually any injured tissue. In Regenerative Medicine, to aid in the repair of cartilage injuries typical of osteoarthritis, as well as chondral injuries in young people. In addition to their use in sports medicine for the treatment of muscle, tendon, or ligament injuries.
The process of obtaining the sample must be performed in the operating room under anesthesia, so a recovery period of about 24 hours is required. Sometimes it is used as an adjuvant treatment alongside another surgical procedure, so the recovery time will depend on the type of surgery performed (usually arthroscopy).
The process of extracting the MSCs is performed by the specialist surgeon in the operating room. The patient’s own fat or bone marrow can be used as donor tissue. It is a relatively quick technique that requires minimal sedation in most cases. These cells are then processed and injected into the patient’s exact injured area for regeneration. After the procedure, the patient can be discharged from the hospital on the same day.

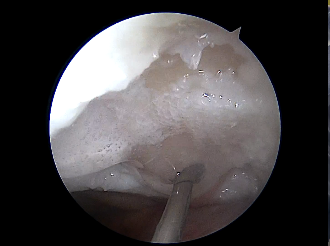
Biological Cartilage
In this The procedure does not use the patient’s own cells, but uses pure acellular collagen. It is a collagen matrix that completely fills the joint defect so that the patient’s own cells can grow and create new, healthy cartilage tissue. This means that only one arthroscopy (minimally invasive surgery) is needed to perform the procedure.
It is an extracellular matrix composed of acellular type I collagen. The collagen is injected into the damaged area, allowing the patient’s own cells to stimulate the creation and growth of cartilage cells in a short amount of time. The product’s great versatility stands out, as it can be used in any type of joint. After implantation, the collagen gel must solidify to increase its resistance to impact (a process that takes about 3-4 weeks).
They are used in any type of focal and localized chondral lesion (cartilage lesion). It is indicated for osteochondral injuries in young and active patients.
The collagen implantation is performed through minimally invasive surgery (usually arthroscopy). After the surgery, a period of rest and joint immobilization is necessary for the first 3-4 weeks (the gel solidification period).
The procedure is performed by the specialist surgeon in the operating room. In the first part of the surgery, the lesion is curetted to remove the damaged cartilage and prepare the site for the future implantation of the collagen. This procedure is usually performed arthroscopically (depending on the type of injury). Next, the collagen gel is implanted and adheres to the injured area. This surgery is performed on an outpatient basis and does not require hospitalization.